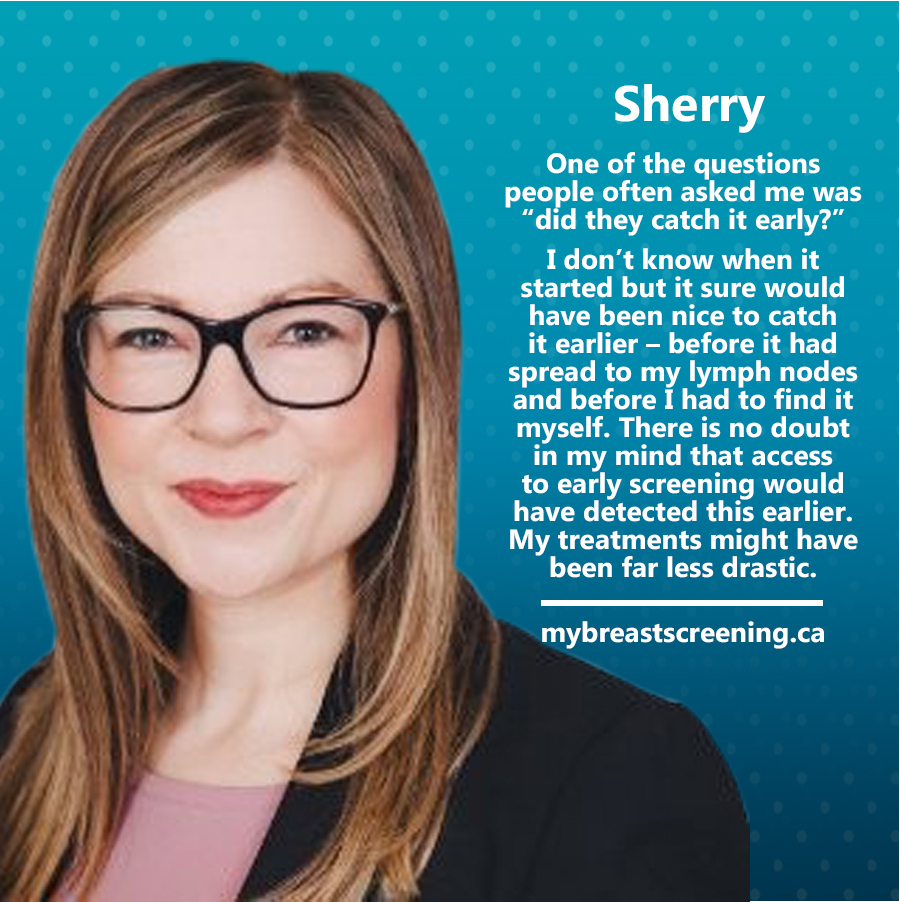
Sherry’s Story
June 8, 2023
Previous Stories
My name is Sherry Wilcox. I am 45 years old and I was diagnosed with breast cancer last year at the age of 44.
I recall asking about a mammogram when I turned 40 and was told by my family doctor that I was too young, that my breasts were too dense, and that screening didn’t start until I turned 50 anyways. And with that, I parked the topic of mammograms until early last year when, at the age of 44, I felt a small lump in my right breast very close to my underarm. I scheduled an in-person doctor’s appointment and my physician suggested it was likely a benign fibroadenoma. That was reassuring, of course, but I requested a mammogram and was told the same thing I was told when I was 40: that I was too young, that my breasts would be too dense and, consequently, that they likely wouldn’t see anything anyways. After pushing a bit more during that same appointment, my doctor agreed to send me for an ultrasound.
After the ultrasound, my physician called me to tell me that there was something slightly suspicious but that I should go for another ultrasound in 16 weeks to confirm stability. In my mind, 16 weeks was too long to wait and it was at that point that I demanded a mammogram and advised her that if she wouldn’t provide me with a requisition, I would go elsewhere. She agreed and ultimately provided me with a requisition. After I had my mammogram, in June of 2022, I got an unexpected phone call about three to four days later. I can remember being in my office downtown and my family doctor advised me over the phone that the radiology report indicated I had breast cancer. I remember her quoting the words from the radiology report when I asked her to read it to me and it said “most definitely invasive carcinoma.”
I remember my head spinning, tears running down my face, being all alone in my office. But I had to shake it off because I needed to take notes and figure out next steps. Over the course of the next several weeks, I would go for a total of four biopsies for different areas of concern. After my first biopsy, my diagnosis of invasive ductal carcinoma for the primary tumor was confirmed and we also learned through the pathology report on a fine needle aspiration of my lymph nodes that the cancer had already spread to at least one lymph note. Shortly thereafter, we learned that my cancer was triple positive: ER, PR and HER2 positive. My tumour was aggressive and in light of my age and the fact that it had already spread to my lymph nodes, the recommended protocol was neoadjuvant chemotherapy, surgery, targeted therapy (because I am HER2 positive) and radiation.
I was in chemotherapy from July to November last year and in December 2022, I had a bilateral mastectomy and a sentinel lymph node biopsy. In early January, upon receipt of the surgical pathology report, we learned that I had not achieved what is known as PCR. There was a small residual amount of cancer left in the tissue that had been removed and since this increased my risk of recurrence, they advised me that I would need to have more treatment: this time a targeted chemotherapy. This protocol would be another 42 weeks, though I got to take a short break in February and March so I could complete my radiation treatments. As it currently stands, I’m still in chemo and will finish up in late October. After that, I’ll have another breast reconstruction surgery, and I’ll continue for the next 5-10 years on some form of hormone blocking treatment to push me into menopause.
So that’s kind of an abbreviated summary of my life as a breast cancer patient in the past year but I’m much more than just a patient. I’m married to Joe, my husband of 18 years, and I’m a mother to three beautiful girls: Niamh, age 12, and our 9-year-old twins, Grace, and Clare. In my spare time, I work full-time as a corporate lawyer and chief compliance officer. My daughters are busy with sports and school and homework, so it would be an understatement to say that my plate was full before being diagnosed. While I have many blessings, including an incredibly supportive employer, I have many people depending on me.
My family has been through hell the past year – watching me so sick has been incredibly difficult for them and I know there have been many times when they have been very scared. I wanted to share a few vignettes with you:
· Our 12-year-old daughter Niamh, who is mature beyond her years in many ways, took control of my surgical drains after my mastectomy. She would drain them and measure output and record the output on a chart.
· Similarly, Grace, one of our twin daughters, was concerned that Joe wouldn’t wake up to help me with meds overnight and decided to take charge and had a schedule in a notebook beside the bed. She would wake up in the middle of the night to help me with meds and then go back to bed and then head off to school the next day.
While these stories are cute and show how capable and caring they are, when I reflect on it further, those were big responsibilities, problems and worries that they were going to school with every day.
I would be remiss without saying that my diagnosis and treatment have changed my life in every possible way.
Physically, I hadn’t fully appreciated how drastic the impact of the outward physical manifestations of this disease would be. From hair loss, to weight gain, to extreme fatigue, to excruciating bone pain…and don’t forget the mastectomy as well as the removal of lymph nodes. The fact that many people no longer even recognize me is a gut-wrenching blow each and every time it happens.
Emotionally, I don’t have enough time to talk about the emotional and psychological impacts of this disease but what I can say is that it is very scary and can be dark and isolating at times. The fear of your children potentially losing a parent far too early can be all-consuming. I found it overwhelming work with a child psychiatrist to help parent your kids through the various anxiety that comes along with an experience like this.
Financially – on this point, I’m incredibly lucky but I am acutely aware of the fact that not everyone enjoys the same privilege that I do in this regard. Through the course of my treatments, I have met so many women undergoing treatment and I can say that these drastic treatments render most unable to work. A sudden loss of income and the inability to pay for life’s basic needs creates a huge financial burden and is a source of great stress for many. I remember being in absolute shock when I found out that one of my recommended immunotherapy drugs, Perjeta, would cost about $75k for the year and that it was not OHIP covered and it was unlikely it would be covered by my group insurance plan. I watched a woman beside me in the chemo room having TCH instead of TCHP and I immediately knew why. That was nothing short of heartbreaking to me because this drug improves prognoses and increases survival rates.
One of the questions people often asked me was “did they catch it early?” I usually don’t answer in any level of detail because, here’s the thing: I don’t know when it started but it sure would have been nice to catch it earlier – before it had spread to my lymph nodes and before I had to find it myself. There is no doubt in my mind that access to early screening would have detected this earlier. My treatments might have been far less drastic.
That was my story and there are so many more out there. I don’t want other women and families to go through what we have endured.
